Korea should learn from best practices to address healthcare crisis
Korea should learn from best practices to address healthcare crisis
Posted October. 24, 2024 08:22,
Updated October. 24, 2024 08:22

The Korean government’s rationale for increasing medical student admission by 2,000 is to promote essential medical care and medical care in rural areas. Securing adequate medical staff in fields directly related to life and addressing gaps in medical access between regions are major medical policy goals in any country. However, the countries researched by a Dong-A Ilbo reporting team, including the United States, Japan, Canada, and the Netherlands, haven’t experienced self-destructive legislative conflicts like Korea while pursuing their policy. This is due to a reasonable compensation system preventing the concentration of medical resources and a gradual increase in the number of doctors per remote region.
The United States offers generous benefits to doctors in essential medical care. The highest salaries for specialists are in neurosurgery and thoracic surgery, with an average annual salary of 1.054 billion won and 995 million won, respectively, which is in stark contrast with Korea, where so-called non-essential fields of dermatology, ophthalmology, plastic surgery, and orthopedics dominate top salaries. The filling rate for essential medical care departments in the United States is 100% (38% in Korea) for thoracic surgery, 99.6% (63% in Korea) for obstetrics and gynecology, and 91.8% (26% in Korea) for pediatrics. The United States also leads the global pharmaceutical market by producing a steady stream of physician-scientists who contribute to improving human health, backed by a compensation system that offers salaries equivalent to clinical doctors.
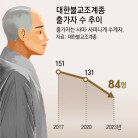
Japan fills the gap in medical access per region by requiring local doctors to work in rural areas for nine years in exchange for support for tuition and living expenses. The system was pilot-run and improved for 38 years in Nagasaki Prefecture before being implemented nationwide in 2008. Japan, facing the challenges of an aging population earlier than Korea, began increasing the medical school student quota early, boosting student quota by 23% over the past 17 years. All the countries researched had an independent body specializing in medical resource estimation and increased student quotas without compromising education quality. It took 20 years for Canada to increase the number of medical school seats by 3,150.
The story is different, however, for Korea. Rather than correcting the compensation system that promotes aesthetic medicine and medical resource concentration in urban areas, the government first attempted to expand the medical school quota. The founding of an independent body to gauge medical resource needs came later. Medical residents in essential care resigned en masse in protest to the government’s unilateral actions. Student quotas for medical schools with poor educational infrastructure have increased significantly, raising concerns. Korea’s healthcare system, known for its excellent, cost-effective service in the world, is on the verge of collapse due to policy failure. The bi-partisan consultative body, which doctors have recently joined, will soon launch operations. We hope for focused attention to help minimize the ramifications of the medical chaos.